How to Help Someone Walk Again
Considering an caused neurologic injury (such as a stroke) affects both sensory and motor function, walking can be severely affected. Sensory changes, weakness, and spasticity bear upon movement strategies, which alter a person's ability to successfully respond to losses of balance. A stroke affects how much and how often a person walks and besides affects walking adaptability—the ability to suit to different weather during ambulation—too as endurance. Gait training generally starts as presently as possible following a stroke, using manual techniques, task-specific training, strengthening, and, when bachelor, body weight-assisted treadmill training and robotic devices.
Movement Strategies Altered past Stroke
A movement strategy or synergy is a flexible, repeatable pattern of motility that can be quickly and automatically accessed by the central nervous system. Movement strategies permit us to shop and reuse patterns of motility that take been successful in the past. Strategies are efficient, automatic move patterns that evolve over time. Each fourth dimension a loss of balance threatens, the nervous organisation draws on these pre-programmed movement strategies to ensure the maintenance of balance.Movement strategies used by the nervous system to respond to perturbations are diminished post-obit a stroke.
Ankle Sway
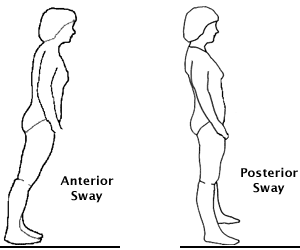
The talocrural joint strategy is used in response to small perturbations is also called ankle sway. Source: Lauren Robertson.
The ankle strategy—also called talocrural joint sway—is used in response to small perturbations or losses of balance. When a small loss of balance occurs—equally when standing on a moving jitney—the foot acts as a lever to maintain rest by making continuous automatic adjustments to the movement of the bus. When a pocket-sized residuum adjustment is needed, muscles close to the floor (anterior tibialis and gastrocnemius) activate starting time and flow upwardly in a distal to proximal pattern.
When a perturbation is too large to be successfully handled by the talocrural joint strategy, the hip strategy is needed. When the hip strategy is used, move is centered about the hip and ankle muscles (inductive tibialis and gastrocnemius) are almost silent. The muscles in the trunk activate first as activation flows downwards to the legs in a proximal to distal pattern. And so, if the bus stops suddenly and the body bends forward, the low back and hamstrings will contract in that society to render the body to upright.
If the perturbation is strong and your center of gravity moves well past your base of support, it is necessary to accept a forward or backward footstep to regain balance. This is referred to every bit a stepping strategy. Studies have shown age-related changes in stepping in older adults. Compared to younger people, older adults initiate the stepping strategy in response to smaller losses of rest and tend to take several minor steps rather than one larger step (Maki & McIlroy, 2006).
Arm movements have a considerable function in balance control and are function of the strategies discussed above. The upper limbs first to react at the very start of a disruption of remainder and continue to be active as the trunk attempts to regain control. By automatically reaching and grasping for support, the arms perform a protective part. In the case of a modest perturbation, upper limb movements can prevent a fall past shifting the heart of gravity away from the imbalance.
When upper extremity paresis or spasticity is present, mail stroke subjects showroom poor protective reactions during a perturbation of balance. They demonstrate a arrears in anticipatory and reactive postural adjustments. These impairments of the affected upper limbs limit a person's ability to recover from perturbations during functional tasks such as walking (Arya et al., 2014).
Even in the absence of a neurologic disorder, historic period-related changes affect upper extremity reaction time when balance is disrupted. Older adults reach for back up surfaces more readily than younger adults but the reach-reaction time is slower. Increased tendency to reach for back up and a slowing of these reactions take been found to exist predictive of falling in daily activities (Maki & McIlroy, 2006).
Comparing Reflexes, Automated Reactions, and Volitional Movement
Reflexes
Remember for a moment that you lot are cooking dinner and accidentally touch on a scalding hot fry pan. You lot experience the heat and withdraw instantaneously. You aren't thinking "I better take my hand off the hot pan before it burns me"—your reflexes take care of that for you. The withdrawal is almost instantaneous because your nervous system senses danger and reflexively withdraws.
Automatic Reactions
This type of reaction is used in movement strategies; they are slower than reflexes simply faster than volitional movement. They are fast enough to help u.s. respond to losses of residue without having to think.
Volitional Motion
This type of motion requires thought and is relatively ho-hum compared to reflexive and automated move. Using our brains to think about movement isn't very practical when we need something done actually fast—by the fourth dimension your brain warns you to bend your waist, step forward, or grab onto something when the motorbus stops abruptly, information technology's already also late to regain balance.
Activeness
Stand upwardly side by side to your chair. Brand sure y'all are standing on a flat, firm surface. Now close your eyes. Notice that your body sways a piffling—you are using the ankle strategy to stay balanced. Notice likewise that after a short corporeality of time you sway less—that ways your nervous system is adjusting. Often, post-obit a stroke, a person looses the ability to use the talocrural joint strategy. This can have a profound bear on on residue.
Stand up again. Ask someone to give yous a little nudge from backside. Try not to take a step. If it was a truly small nudge you will probable bend at the waist to try to regain your remainder. This is an example of the hip strategy.
Now ask your partner to give you lot a slightly bigger nudge from backside. If the nudge is big enough you'll take to take a step. This is the stepping strategy.
We utilize these strategies automatically, all day long, without try. Someone who has had a stroke can't access these strategies as rapidly as you can. If faced with a nudge from a passerby, or a bus
Importance of Walking Early and Oftentimes
Regaining the power to walk following a stroke is of paramount importance to patients and caregivers alike; improving balance and walking leads to greater independence and improves full general well-being.
In the first week following a stroke, simply one-third of patients are able to walk without assistance. In the following weeks, walking power by and large improves. At iii weeks, or at hospital discharge, more half of stroke survivors can walk unaided. By 6 months, more than 80% are able to walk independently without concrete assistance from some other person (Balasubramanian et al., 2014).
Following a stroke, walking tin can take a lot of energy; impaired muscle office, weakness, and poor cardiovascular workout can double the amount of energy expended. The loftier energy cost of walking can affect a person'due south ability to participate in daily activities and lead to a vicious wheel where physical activity is avoided. For example, in one study, stroke patients walked fifty% of the daily amount of matched sedentary adults and used 75% of their VO2 peak for walking at a submaximal charge per unit (Danielsson et al., 2011).
Walking may improve more rapidly when patients are involved in setting specific goals. The results of several motor learning studies in which the person'southward attention was focused on the outcome of an action rather than the activeness itself produced more effective functioning than focusing on the quality of the move (Carr & Shepherd, 2011).
In the infirmary, an early goal for walking might exist to walk to the side by side appointment, or to walk at least office of the way, rather than being transported in a wheelchair. Each day the patient should be encouraged to select a altitude to walk independently and safely. Initially, this may be but a few steps. The goal is to walk the chosen distance a certain number of times a solar day, increasing altitude as soon every bit possible, and keeping a tape of progress, which gives the patient a specific focus (Carr & Shepherd, 2011).
Walking Adaptability, Stepping, and Postural Control
Walking is greatly dependent upon our power to adapt to varying environmental conditions and tasks. Walking from the bedroom to the bath with a walker requires a unlike level of attention and adaptability than walking across a decorated street carrying a purse of groceries. Fifty-fifty walking and talking tin can be a challenge for post stroke patients.
Over time, up to 85% of individuals with a stroke regain independent walking ability, but at belch from inpatient rehab only near vii% can manage steps and inclines or walk the speeds and distances required to walk competently in the customs. Limited ability to adjust to changes in the chore and environment means a person either avoids walking in complex situations (a safety strategy) or has a heightened risk of falls when required to walk under these challenging conditions (Balasubramanian et al., 2014).
Despite its importance, assessment of walking adjustability has received relatively piddling attending. Often used assessments of walking ability after stroke involve walking short distances (such every bit the Timed Up and Go test) and examination of isolated limb movements (such as the Fugl-Meyer Assessment). Although valuable, these assessments do not take into business relationship the skills needed to re-appoint in prophylactic and independent airing in the home and community. Comprehensive assessments and specific interventions are needed to improve walking adaptability (Balasubramanian et al., 2014).
In addition to the ability to accommodate to different conditions and tasks, walking adaptability has two other requirements: (1) stepping, and (2) postural control (Shumway-Cook & Woollocott, 2012). Stepping involves the ability to generate and maintain a rhythmic, alternate gait pattern as well as the ability to start and stop. Postural control involves both the musculoskeletal and nervous systems.
To walk finer, the central nervous system must:
- Generate the basic stepping design of rhythmic reciprocal limb movements while supporting the body against gravity and propelling it frontwards.
- Maintain control of posture (equilibrium) to keep the centre of mass over a constantly moving base of support and maintain the torso upright in infinite.
- Adapt to environmental circumstance or changes in the behavioral goal (Balasubramanian et al., 2014).
These components are especially necessary for complex tasks. For instance, walking adaptability is crucial on uneven footing or cluttered terrains and when the chore requires walking and turning or negotiating a curved path. At that place are endless combinations of task goals and ecology circumstances that must be considered to comprehensively capture walking adaptability (Balasubramanian et al., 2014).
Walking adjustability is very of import for community ambulation. Patla and Shumway-Cook have described "dimensions" that affect a person's ability to adapt while walking. These are external demands that must be met for successful community mobility:
- Distance (distance walked)
- Temporal factors (fourth dimension needed to cross a busy street or crosswalk, power to maintain the same speed every bit those around them)
- Ambience conditions (rain, heat, snow, etc.)
- Physical load (packages carried, number of doors that need to be opened)
- Terrain (stairs, curbs, slopes, uneven ground, grass, elevators, obstacles)
- Attentional demands (distractions in the environs, noise, cars, crowds, talking)
- Postural transitions (stopping, reaching, backing upwards, turning head, change management)
- Traffic density (number of people within arm'due south reach, unexpected collisions and near collisions with other people) (Shumway-Cook et al., 2002)
Improving Endurance for Walking
Information technology is evident that many patients are discharged from inpatient rehabilitation severely deconditioned, significant that their free energy levels are too low for agile participation in daily life. Physicians, therapists, and nursing staff responsible for rehabilitation practice should address this issue not simply during inpatient rehabilitation but as well after discharge by promoting and supporting customs-based exercise opportunities. During inpatient rehabilitation, group sessions should be frequent and need to include specific aerobic training. Physical therapy must take advantage of the training aids available, including exercise equipment such as treadmills, and of new developments in computerized feedback systems, robotics, and electromechanical trainers.
Janet Carr and Roberta Sheperd
University of Sydney, Australia
Although many people affected past stroke accept regained some ability to walk by the time they are discharged from rehab, many have low endurance, which limits their power to perform household tasks or even to walk short distances. After a stroke, walking requires a much higher level of energy expenditure, and upon discharge many stroke patients are not necessarily functional walkers (Carr & Sheperd, 2011).
Functional walking is assessed using tests of speed, distance, and time. Minimal criteria for successful community walking include an independent walking velocity of 0.8 m/south or greater (about ii.6 feet/second), the ability to negotiate uneven terrain and curbs, and the physical endurance to walk 500 meters or more. In a review of 109 people discharged from concrete therapy, simply 7% achieved the minimum level. Cardiorespiratory fitness training can address both the efficiency with which people affected by stroke can walk and the distance they are able to achieve (Carr & Sheperd, 2011).
The loss of independent ambulation outdoors has been identified every bit one of the nigh debilitating consequences of stroke. Among stroke survivors 1 yr after stroke, the most striking area of difficulty was depression endurance measured by the distance walked in a vi-minute walk examination. Those subjects able to complete this test were able to walk on average only 250 meters (820 anxiety) compared to the age-predicted distance of >600 meters (virtually 2,000 anxiety), equivalent to 40% of their predicted ability and non far enough for a reasonable and active lifestyle. The detrimental issue of low exercise capacity and musculus endurance on functional mobility and on resistance to fatigue is likely to increase subsequently discharge if follow-up physical action and exercise programs are not bachelor (Carr & Sheperd, 2011).
In 2002 the American Thoracic Society (ATS) published guidelines for the 6-infinitesimal walk examination with the objective of standardizing the protocol to encourage its further application and to allow direct comparisons among different studies and populations. The American Thoracic Guild guidelines include test indications and contraindications, safety measures, and a step-by-footstep protocol as well every bit aid with clinical interpretation (Dunn et al., 2015).
Key components of the protocol include the test location, walkway length, measurements, and instructions. According to the American Thoracic Society protocol, the test should be performed on a flat, enclosed (indoor) walkway xxx m (simply under 100 anxiety) in length. This protocol requires 180° turns at either stop of the walkway and additional infinite for turning. The guidelines advise that shorter walkway lengths require more directional changes and tin can reduce the distances achieved. The influence of directional changes may be amplified in the stroke population, who characteristically have impaired remainder, asymmetric gait patterns, and contradistinct responses for turn training. Conversely, reducing the number of directional changes may increment the altitude achieved (Dunn et al., 2015).
Torso Weight-Supported Treadmill Training
Body weight-supported treadmill training (BWSTT) is an increasingly being used to encourage early on walking following a stroke. It is a rehabilitation technique in which patients walk on a treadmill with their body weight partly supported. Body weight-supported treadmill training augments walking by enabling repetitive practice of gait (Takeuchi & Izumi, 2013).
In patients who have experienced a stroke, partial unloading of the lower extremities past the body weight-support system results in straighter trunk and human knee alignment during the loading phase of walking. It can also better swing1 disproportion, pace length, and walking speed, and allows a patient to practice nearly normal gait patterns and avoid developing compensatory walking habits, such as hip hiking and circumductiontwo (Takeuchi & Izumi, 2013).
1 Swing stage of gait: during walking, the swing stage begins as the toe lifts of the footing, continues as the knee bends and the leg moves forward, and ends when the heel come in contact with the footing.
2 Circumduction: a gait aberration in which the leg is swung around and forward in a semi-circle. The hip is ofttimes hiked up to create enough room for the leg to swing forward.

Example of a body-weight supported treadmill. Source: NIH, 2011.
Treadmill walking allows for independent and semi-supervised practise, for those with more power, as well as improving aerobic capacity and increasing walking speed and endurance. The very early practice of assisted over-ground and harness-supported treadmill walking is probably disquisitional to good postal service-discharge functional capacity in terms of both performance and free energy levels (Carr & Shepherd, 2011).
The Locomotor Experience Applied Post Stroke (LEAPS) trial—the largest stroke rehabilitation study ever conducted in the United States—set out to compare the effectiveness of the torso weight-supported treadmill grooming with walking practice. Participants started at two dissimilar stages—ii months post stroke (early locomotor training) and half dozen months post stroke (late locomotor preparation). The locomotor preparation was besides compared to a home exercise program managed by a concrete therapist, which was aimed at enhancing flexibility, range of movement, forcefulness, and residue equally a way to ameliorate walking. The primary measure was improvement in walking at ane twelvemonth after the stroke (NINDS, 2011).
In the LEAPS trial, stroke patients who had physical therapy at dwelling improved their ability to walk just every bit well as those who were treated in a training program that requires the use of a torso weight-supported treadmill device followed by walking practice. The study, funded past the NIH, too found that patients connected to ameliorate up to 1 twelvemonth after stroke—defying conventional wisdom that recovery occurs early and tops out at 6 months. In fact, even patients who started rehabilitation as late as 6 months after stroke were able to improve their walking (NINDS, 2011).
"We were pleased to see that stroke patients who had a domicile physical therapy exercise program improved simply as well as those who did the locomotor grooming," said Pamela W. Duncan, principal investigator of LEAPS and professor at Knuckles Academy School of Medicine. "The home physical therapy program is more than convenient and pragmatic. Usual care should comprise more intensive exercise programs that are easily accessible to patients to improve walking, role, and quality of life."
Robotic Gait Training Devices
Several lower-limb rehabilitation robots have been developed to restore mobility of the affected limbs. These systems can exist grouped according to the rehabilitation principle they follow:
- Treadmill gait trainers
- Foot-plate-based gait trainers
- Over-ground gait trainers
- Stationary gait trainers
- Talocrural joint rehabilitation systems
- Stationary systems
- Active pes orthoses (Díaz et al., 2011)
The Lokomat System

Source: Diaz et al., 2011.
Many robotic systems have been adult aiming to automate and improve body weight-assisted treadmill trainers as a means for reducing therapist labor. Usually these systems are based on exoskeleton type robots in combination with a treadmill. 1 such system—the Lokomat—consists of a robotic gait orthosis and an advanced body weight-back up system, combined with a treadmill. It uses computer-controlled motors (drives) that are integrated in the gait orthosis at each hip and knee joint joint. The drives are precisely synchronized with the speed of the treadmill to ensure a precise match between the speed of the gait orthosis and the treadmill (Diaz et al., 2011).
The LokoHelp is another device developed for improving gait afterwards brain injury. The LokoHelp is placed in the middle of the treadmill surface, parallel to the walking direction and fixed to the front of the treadmill with a uncomplicated clamp. It also provides a trunk weight-support system. Clinical trials have shown that the organization improves the gait ability of the patient in the same fashion as the manual locomotor preparation; however, the LokoHelp required less therapeutic assist and thus therapist discomfort is reduced. This fact is a general decision for almost all robotic systems to date (Díaz et al., 2011).
Over-ground gait trainers consist of robots that assist the patient in walking over footing. These trainers permit patients to movement under their own command rather than moving them through predetermined motility patterns. The KineAssist is one robotic device used for gait and balance preparation. Information technology consists of a custom-designed torso and pelvis harness attached to a mobile robotic base of operations. The robot is controlled according to the forces detected from the subject by the load cells located in the pelvic harness (Díaz et al., 2011).
The ReWalk Robotic Suit

Source: Diaz et al., 2011.
ReWalk is a wearable, motorized quasi-robotic suit that can be used for therapeutic activities. ReWalk uses a light, wearable caryatid support adjust that integrates motors at the joints, rechargeable batteries, an array of sensors, and a computer-based control arrangement. Upper-body movements of the user are detected and used to initiate and maintain walking processes (Díaz et al., 2011).
The capacity of robots to deliver high-intensity and repeatable preparation make them potentially valuable tools to provide high-quality treatment at a lower cost and attempt. These systems can likewise exist used at home to permit patients to perform therapies independently, not replacing the therapist just supporting the therapy program. However, despite the bewitchery of robotic devices, clinical studies yet show little evidence for the superior effectiveness of robotic therapy compared to current therapy practices, although robotics have been shown to reduce therapist effort, time, and costs (Díaz et al., 2011).
Source: https://www.atrainceu.com/content/12-regaining-ability-walk
0 Response to "How to Help Someone Walk Again"
Postar um comentário